Striking South African doctors pose a serious threat to the human rights of all of the country’s residents -- even refusing to treat emergency cases…’
June 21 2009 – CAPE TOWN. For the third time within two months, the country’s 18,000 overworked, underpaid and totally demoralised public hospital doctors are planning yet another wildcat strike from Monday at the 640 state hospitals. They start the strike in KwaZulu-Natal and the Eastern Cape on Monday, and it will expand to the other provinces Tuesday and Wednesday.
For the third time within two months, the country’s 18,000 overworked, underpaid and totally demoralised public hospital doctors are planning yet another wildcat strike from Monday at the 640 state hospitals. They start the strike in KwaZulu-Natal and the Eastern Cape on Monday, and it will expand to the other provinces Tuesday and Wednesday.
The SA Medical Association spokesman Lebogang Phahladira told the Sunday Times on Saturday that the striking doctors ‘will report for duty and sign attendance registers – but will refuse to treat patients, even in emergencies.”
And South Africa no longer has enough doctors in the private sector nor in the military to help out in emergencies– even if they were asked. South Africa now only has about one doctor for every 200,000 people and its public hospitals are overburdened due to the combined TB-AIDS epidemics.
In 1985, South Africa’s public health service had more than 25,000 physicians and dentists; 5,100 specialists, 222 dental specialists and 18,700 paramedical workers, registered at the South African Medical and Dental Council; and 155,000 registered and staff-nurses. South Africa is in the midst of the world’s most devastating co-epidemic of two simultaneous killer-diseases, TB and XDR-TB -- and the rapidly-shrinking medical staff can no longer cope.
“Thousands of patients face being turned away from public hospitals tomorrow (Monday) if the wildcat strike by South Africa’s 18,000 disgruntled state doctors goes ahead”, reports the Sunday Times.
The South African Medical Association (Sama) spokesman Lebogang Phahladira said on Saturday that it ‘’expected a total shutdown” in KwaZulu-Natal and the Eastern Cape, followed by the rest of the country on Tuesday and Wednesday.
- By late Saturday, neither the doctors in the South African National Defence Force nor the private hospital sector — both central to government’s previous strike contingency plans — had received any requests for help.
 Sama spokesman Phahladira said members had “overwhelmingly” decided to strike. Doctors would report for duty and sign attendance registers but would not treat patients. “None of the departments will be operational and we will not see any patients, even in an emergency. We will not work until our demands are met,” said Phahladira.
Sama spokesman Phahladira said members had “overwhelmingly” decided to strike. Doctors would report for duty and sign attendance registers but would not treat patients. “None of the departments will be operational and we will not see any patients, even in an emergency. We will not work until our demands are met,” said Phahladira.
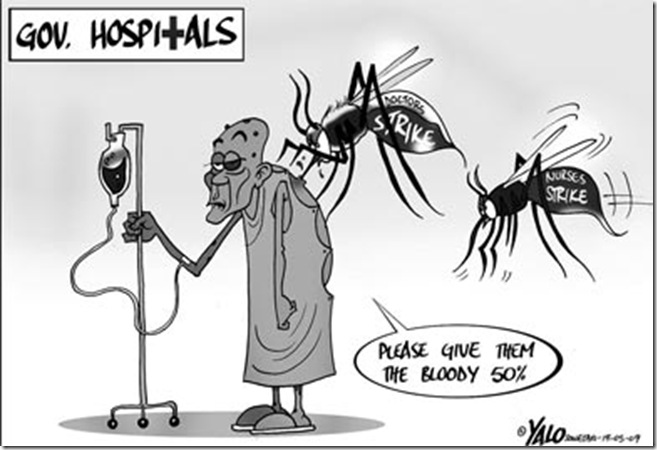
Sama wants a minimum 50% salary increase for its 7000-odd members. Government has offered a mere 5% – which is less than inflation. Apparently, a revised deal will be presented at a bargaining council meeting forthcoming Wednesday.
Sama chairman Mac Lukhele said although many members planned to strike, the union had appealed for patience until the outcome of this latest meeting. Some have agreed to hold off on strike action.
- A spokesman for the Hospital Association of South Africa, Kurt Worrall-Clare, said the group had had no requests for help. He said that in the past the association, representing all major private hospitals, had received formal requests from the government at least two or three days before anticipated strikes.
- Morgan Chetty, chairman of the KZN Managed Care Coalition representing some 3,500 doctors in the private sector, said they would not have enough doctors to help out if asked.
- Defence force spokesman Sam Mkhwanazi said the SANDF ‘s medical teams have also had not been asked to assist.
‘There is no crisis’ - KwaZulu-Natal health MEC…
The KwaZulu-Natal provincial MEC for health, Sibongiseni Dhlomo, told the Sunday Times yesterday ‘the department did not believe outside assistance was necessary because there was no crisis.’ However, in Gauteng on Friday, a provincial memo to Johannesburg hospitals requested contingency plans be put in place and strike committees set up. Gauteng health spokesman Mandla Sidu said it was the “prerogative” of hospital chief executives to request SANDF and private sector assistance. Western Cape health spokesman Faiza Steyn said the province had a “sufficient pool” of doctors, including part-time doctors, military doctors and agency staff, to draw from. Attempts this week to get comment from the national Department of Health were unsuccessful. — Additional reporting by Chandre Prince http://www.thetimes.co.za/PrintEdition/Article.aspx?id=1021082
Nightmare scenario
 During the previous wild-cat strikes on June 6, 2009 and May 29 2009, accident victims who were rushed to state hospitals in Pretoria had to wait for three days for emergency surgery, and in Cape Town, it was reported that during a protest march on Parliament, a petition was handed in by more than 100 local doctors, pharmacists and other public sector health professionals – demanding fair pay and better working conditions. The march was organised by the SA Medical Association (Sama). The document calls for the immediate implementation of the promised Occupational Specific Dispensation, which was supposed to take effect in July last year; a minimum 50 percent increase in basic salary; and the unfreezing of all essential public sector medical posts. At the moment, more than 60% of the nursing staff posts also remain because there simply aren’t enough qualified people to fill them.
During the previous wild-cat strikes on June 6, 2009 and May 29 2009, accident victims who were rushed to state hospitals in Pretoria had to wait for three days for emergency surgery, and in Cape Town, it was reported that during a protest march on Parliament, a petition was handed in by more than 100 local doctors, pharmacists and other public sector health professionals – demanding fair pay and better working conditions. The march was organised by the SA Medical Association (Sama). The document calls for the immediate implementation of the promised Occupational Specific Dispensation, which was supposed to take effect in July last year; a minimum 50 percent increase in basic salary; and the unfreezing of all essential public sector medical posts. At the moment, more than 60% of the nursing staff posts also remain because there simply aren’t enough qualified people to fill them.
Three-day wait in trauma unit for surgery:
Nurses and doctors at the Pretoria Academic Hospital, which was renamed the Steve Biko hospital in 2008, told the emergency-room patients waiting for their emergency surgery on June 6 that ‘it was out of their control about who gets to be operated when, we are overloaded with work’, telling patients that they were so permanently understaffed that emergency patients were forced to wait for days, with wounds remaining undressed and infections setting in, even without any strike actions…. For instance, emergency cases rushed to this academic hospital now already are being forced to wait without treatment in the trauma department of the Pretoria Academic Hospital for at least three days before they can be operated on. http://jv.news24.com/Beeld/Suid-Afrika/0,,3-975_2527110,00.html
--------------------------------------------------------------------------------------------------------------------------------
Best public health system on African continent only fifteen years ago…
South Africa used to have the best Western public-health system on the African continent: In 1985, South Africa’s public health service had more than 25,000 physicians and dentists; 5,100 specialists, 222 dental specialists and 18,700 paramedical workers, registered at the South African Medical and Dental Council, and more than 127,000 registered nurses signed up at the Nursing Council – and by 2002, there were 155,000 nurses.
In 2002, Statistics SA showed that the country had 155,000 top-trained practicing nurses, for a nurse/population ratio of about 343 per 100,000, well above the 200 per 100,000 minimum required by the World Health Organization. Now, the country’s public hospitals show a severe staffing problem, with more than 60% of all the nursing posts countrywide remaining vacant for months on end. In many rural towns in all the South African provinces, there no longer are any physicians at all.
- In other areas there are clinics, but even the most basic medications are lacking. http://jv.news24.com/Beeld/Wereld/0,,3-71_2527071,00.html
- Also: Afrikaner doctor chosen Saskatchewan Physician of the Year 2009
--------------------------------------------------------------
There had also been a public service strike in June 2007, which included all the nursing-, technical-, clerical and janitorial staffers in the country’s public hospitals -- but which at that time, had seen doctors keeping themselves aloof from striking –, although they often publicly did sympathise with the poor working conditions of the medical staff. And when the nursing staff did not get the pay rises they wanted even after this devastating strike, during which many people died because they were left untreated in emergency rooms, they left the public service enmasse. Now there’s a an average, countrywide nursing shortage of 60%, with some public hospitals reporting up to 90% shortages.
Cosatu president Sidumo Dlamini said the state of staffing at the country’s public hospitals was a "ticking time bomb" and noted that if doctors were not happy in South Africa, the entire country would suffer.
- "We are saying to our government that this matter is very urgent. Workers in this country have been in recession for many, many years. When salaries get lower, it is destroying the country," he said.
36 hour shifts for $800 a month, overtime without pay :
The doctors’ two-month campaign for better working conditions also include weeks of angry picketing . Doctors warn that they are being grossly underpaid, are forced work 36-hour shifts without any overtime pay because of the severe shortage of physicians and specialists, that there also is an often dramatic shortages of critical drugs and equipment at all the state hospitals, and heavy workloads for physicians, with shifts lasting up to 36 hours. The government had moreover offered these doctors a deeply insulting 5% in a pay-rise, which does not even cover inflation, said the South African Medical Association chairwoman Denise White.
The Health Professions Council of SA refuses to support the strike – albeit does ‘acknowledge the need for adequate remuneration packages”.
- "We do not support or condone the strike by public sector doctors over salaries and working conditions as they provide an essential service. However we fully acknowledge the urgent need for commensurate remuneration packages and improved working conditions," said HPCSA Registrar and CEO, advocate Boyce Mkhize. "Public sector doctors are professional health care practitioners working under sometimes extremely challenging conditions while saving lives on a daily basis and should be remunerated accordingly."
Doctors, nurses fleeing overseas:
HPCSA statistics indicate that over the past year 3,550 certificates of good standing were issued for medical practitioners alone while 22,032 certificates were issued since 1 April 2003. The majority of these certificates are requested by doctors applying for positions overseas.
--------------------------------------------------------------------------------------------------------------------------------
Medical staff also on strike in June 2007
There had also been a public service strike in June 2007, which included all the nursing-, technical-, clerical and janitorial staffers in the country’s public hospitals -- but which at that time, had seen doctors keeping themselves aloof from striking –, although they often publicly did sympathise with the poor working conditions of the medical staff. And when the nursing staff did not get the pay rises they wanted even after this devastating strike, during which many people died because they were left untreated in emergency rooms, they left the public service enmasse. Now there’s a an average, countrywide nursing shortage of 60%, with some public hospitals reporting up to 90% shortages.
'can a doctor still function safely after a 36-hour shift?’
Interns take home about R8,000 ($800) after deductions and specialists roughly double that, according to the United Doctors Forum deputy chair Mpho Mohlala. "We are not giving proper basic care to the patients. You are not doing justice to the patients. Do you think operating (on) a patient without having sleep for 36 hours, you are functioning? You are non-functional," said Mohlala.
Government denies there’s any crisis
"We've got an exodus of doctors leaving the country, going to work overseas, and we've got lots and lots of doctors moving out of the public sector to the private sector," she told Agence France Presse news agency.
- The health department denies that its sector is in crisis, saying media reports are 'alarmist'.
“Illegal march” – but would they fire all their doctors?
At the moment, more than 60% of the nursing staff posts already are left open. The exodus of South African nurses to Western countries started from 2004 – but the government itself has made matters much worse because it failed to address the complaints issued by staffers ever since the 2007 public service strikes, which brought no improvement in the working conditions. South Africa’s nurses started migrating abroad enmasse. And now, it looks as if South Africa’s doctors are also throwing in the towel – thus condemning Africa’s once so brilliant First-World public health service to death. http://www.news24.com/News24/South_Africa/News/0,,2-7-1442_2523853,00.html
-------------------------------------------------------
History of South African public health service under apartheid:
South Africa’s present public health system was launched by the apartheid-government from 1977. It started an ambitious building programme of public hospitals, outpatient clinics and rehabiliation facilities countrywide for people of all races, and where patients could pay for health care according to their income. The motto of the SA public health service was: “Patients pay according to their income, and those who cannot afford it, get treated for free.” Anyone earning less than R20,000 a year did not pay anything at all – ever, even for the most sophisticated open heart-surgery.
Preventative care was emphasized during apartheid:
The emphasis at these facilities was on preventative care: focussing on the rapid detection and prevention of the huge number of diseases Africa is prone to, from bubonic plague, bilharzia, cholera, tuberculosis, leprosy, polio, smallpox, malaria, haemorrhagic viral diseases, yellow fever, venerial diseases and meningitis.
- Within ten years after launching its public health service programme, South Africa had brought leprosy, yellow fever, smallpox and cholera completely under control, and polio and tuberculosis were 'being well-managed’ because of the enforced, free immunisation of all children of all races against polio and tuberculosis.
By 1985, there were 122,402 beds in 623 state hospitals, and in 1985 the four provinces at that time, spent $23,7million each for maintaining their new public health facilities and clinics. The giant Baragwanath hospital built right next to Soweto’s railway line, added another 120,000 annual in-patients to this list -- as well as treating 1,5-million outpatients a year, serving the entire greater-Soweto area. Its maternity wards, if put end to end, measures a total of 1km. Mamelodi hospital near Pretoria also was added at this time with 12,000 beds, serving the black community for the entire greater-Pretoria region. However all the public hospitals treated patients of all races – albeit they were treated in racialy-segregated facilities during apartheid, which ended officially in 1994.
South Africa’s first-world medical standards also drew calls for help from the rest of Africa: for instance when the greatly feared haemorrhagic Marburg fever broke out in Kenya and the Congo, South African virologists were asked to attend to these emergencies by the World Health Organisation, thus preventing large-scale epidemics.
Health schemes for 5,2-million black taxpayers during apartheid:
The South African government also set up medical-health schemes for the working black population: by the end of 1985, there were 262 such schemes with a total membership of 5.2-million black taxpayers, with the fastest-growing scheme, Bonitas, having a membership of 184,672 members by 1986, mostly black taxpayers in government service, on farms and even in domestic service.
In 1985, South Africa’s public health service had more than 25,000 physicians and dentists; 5,100 specialists, 222 dental specialists and 18,700 paramedical workers, registered at the South African Medical and Dental Council, and more than 127,000 registered nurses signed up at the Nursing Council. Source: ‘This is South Africa,’ Jan 1987, ISBN 0797006540 State Printing Office, Pretoria.
sources, links:
- http://www.news24.com/News24/South_Africa/News/0,,2-7-1442_2524239,00.html
- http://www.samedical.org/index.php?option=com_content&task=view&id=577&Itemid=230
- http://www.samedical.org/
- http://www.nursingadvocacy.org/news/2005jan/14_sa_star.html
- http://www.nursingadvocacy.org/faq/migration.html
- http://www.polokwane.org.za/index.php?readnews+1558
- http://www.rudasa.org.za/student/limpopo/polokwane.php
- http://www.polity.org.za/article/sa-tshabalalamsimang-telemedicine-project-launch-23102007-2007-10-23.
- http://www.iol.co.za/index.php?set_id=1&click_id=13&art_id=nw20080118125902579C182990
- http://www.irinnews.org/Report.aspx?ReportId=72719
- http://www.sowetan.co.za/News/Article.aspx?id=1002506
- http://en.wikipedia.org/wiki/Manto_Tshabalala-Msimang
- http://jv.news24.com/Beeld/Suid-Afrika/0,,3-975_2527110,00.html
- The Citizen- This hospital would have made Biko proud
- Health minister concerned about safety standards at SA hospitals
- Few rural doctors left in South Africa: http://jv.news24.com/Beeld/Wereld/0,,3-71_2527071,00.html
- http://www.thetimes.co.za/PrintEdition/Article.aspx?id=1021082
No comments:
Post a Comment
Note: only a member of this blog may post a comment.